Definition of Normal Sperm Morphology
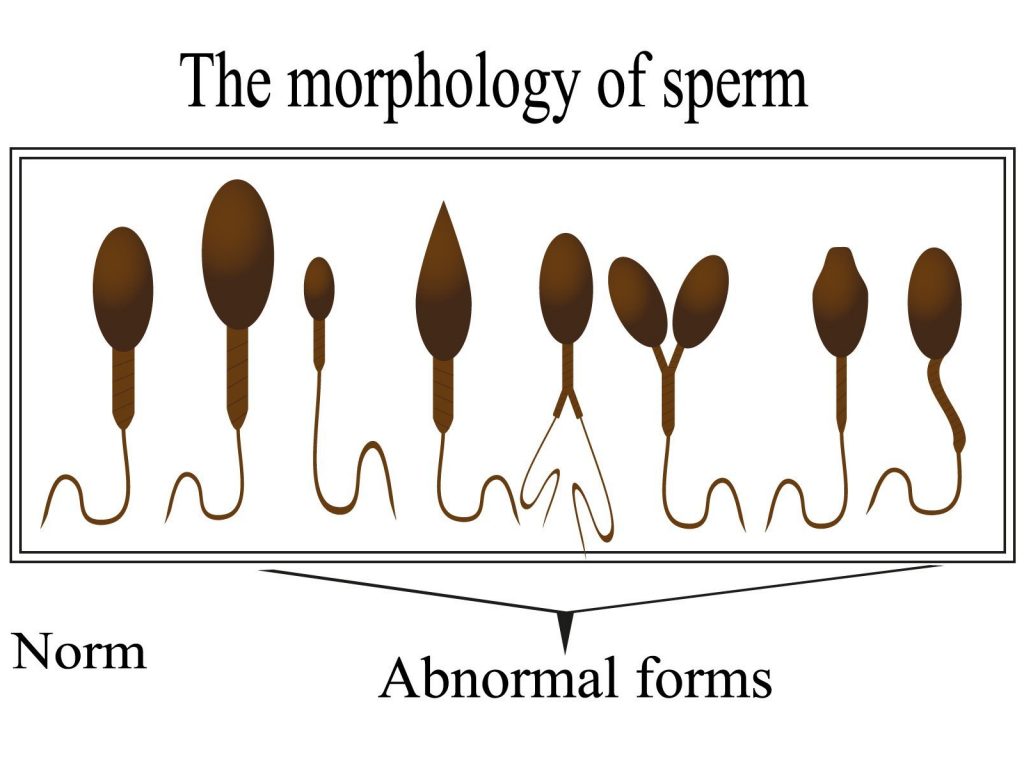
Teratozoospermia (also known as teratospermia) is a condition in which a higher-than-normal proportion of sperm in a semen sample has an abnormal shape or structure. Sperm morphology refers to the size and form of the sperm, which play important roles in sperm movement and the ability to fertilise an egg.
During semen analysis, a portion of the sample is specially prepared to allow sperm structure to be examined under a microscope. This enables the assessment of sperm morphology by identifying the proportion of sperm that meet strict criteria for normal appearance, and categorising abnormalities.
When the percentage of morphologically abnormal sperm falls above recognised reference values, the condition is diagnosed as teratozoospermia. However, morphology results should not be considered in isolation, and are most clinically meaningful when interpreted alongside other parameters, such as sperm count and motility.
WHO Reference Values and Standards
According to the World Health Organisation (WHO)’s morphological criteria, semen quality can be recorded extremely accurately by evaluating head, midpiece, and tail defects. The WHO guidelines simplify this by reporting the percentage of sperm that meet normal morphology criteria.
- A semen sample is considered morphologically normal if at least 4% of sperm fulfil the normal criteria.
- This means a sample could have 96% abnormal forms and still be within the normal range.
- Historically, the WHO had a previous reference value of 6% normal forms, but more recent definitions have reduced this to the current 4%.
Kruger’s Strict Criteria
At Concept Fertility, morphology is scored using Kruger’s Strict Criteria, which is the classification recommended by the WHO.
- Under this system, a cut-off of 4% normal forms is used to distinguish normal from abnormal.
- If a sample does not achieve 4% normal forms, the condition is diagnosed as teratozoospermia.
- This strict method ensures consistent and clinically meaningful reporting of sperm shape within fertility assessments.
Morphology should always be interpreted in context with other semen analysis parameters and clinical history.
Common Causes of Teratozoospermia
Teratozoospermia can arise from a range of medical, physiological, and environmental factors. In many cases, abnormal sperm morphology is linked to conditions that disrupt normal testicular function, increase oxidative stress, or interfere with hormone balance and sperm development.
Often, multiple factors may contribute. Below are some of the most commonly recognised causes.
Varicocele
Varicocele, an enlargement of the veins within the scrotum, is one of the most commonly identified medical causes of abnormal sperm morphology. Research shows that dilated scrotal veins can raise testicular temperature, reduce oxygen supply, and increase oxidative stress, all of which may impair sperm development and structure. Studies have demonstrated poorer morphology in men with untreated varicocele, with some improvement seen following corrective treatment.
Coeliac and Crohn’s Disease
Coeliac disease has been associated with impaired semen quality, including abnormal sperm morphology. Chronic inflammation and malabsorption of key nutrients such as zinc and folate may interfere with normal spermatogenesis. Research suggests that semen parameters may improve in some men after diagnosis and adherence to a gluten-free diet.
Crohn’s disease is another factor that may affect sperm morphology through similar ongoing systemic inflammation, oxidative stress, and nutritional deficiencies. The disease has been linked to altered semen parameters in some studies, highlighting the importance of control and clinical assessment when investigating male fertility.
Lifestyle Factors
Lifestyle and environmental factors are well-recognised contributors to abnormal sperm morphology. Smoking, excessive alcohol intake, obesity, heat exposure, and environmental toxins have all been linked in research to increased oxidative stress and structural sperm abnormalities. In some cases, lifestyle changes may lead to measurable improvements in morphology over time.
Treatment Options
Male factor infertility, including teratozoospermia, can often be successfully managed with modern fertility treatments. All fertility treatment plans are carefully tailored to each individual, taking into account semen analysis results, medical history, and the reproductive goals of both partners. Advances in assisted reproductive technology mean that effective options are often available even when sperm morphology is significantly reduced.
Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection (ICSI) is an advanced fertilisation technique offered as part of an IVF cycle, particularly helpful for couples with sperm-related infertility, such as poor morphology, low motility, or previous fertilisation difficulties. In ICSI, an embryologist selects a single sperm and directly injects it into the cytoplasm of an egg, bypassing many of the biological barriers that may prevent natural fertilisation.
This approach can improve the probability of fertilisation in cases when conventional IVF may be less effective due to sperm-related issues. While ICSI does not guarantee success in every case, it remains one of the most widely used and studied treatments for male factor fertility.
Book a Specialist Consultation
If you have concerns about sperm morphology or male fertility, a specialist consultation can provide clarity, reassurance, and personalised guidance. At Concept Fertility, consultations are led by experienced fertility specialists who can review semen analysis results in detail, explain what they mean for your fertility, and outline appropriate next steps.
Whether you are at the early stages of investigation or considering assisted fertility treatment, expert support can help you make informed decisions with confidence. Book a specialist consultation with Concept Fertility to discuss your individual fertility assessment and treatment options.